For the first time, ambulance crews and urgent care professionals across England can instantly access Treatment Escalation Plans (TEPs) for patients from Devon and Cornwall, wherever and whenever they’re needed.
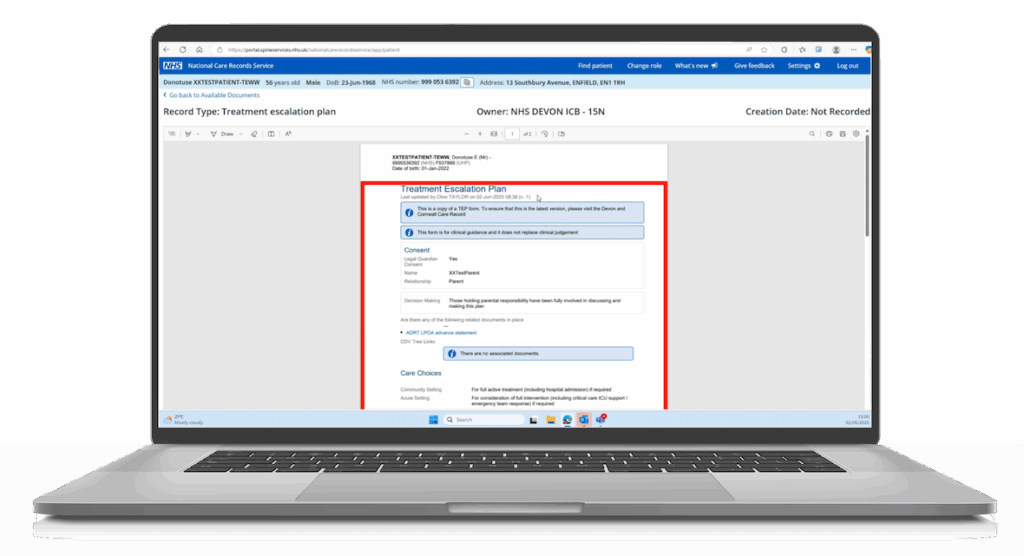
On 2 June 2025, the Devon and Cornwall Shared Care Record (DCCR) began publishing TEPs to the National Record Locator (NRL), making these important care plans discoverable nationally through the National Care Records Service (NCRS). The NCRS provides a quick and secure way for health and care workers to access national patient information.
This milestone removes a major barrier for frontline teams, who previously had to rely on incomplete information when making urgent care decisions. Now, they can see a clear picture of a patient’s wishes in seconds, supporting faster, safer and more compassionate care. For patients and families, it provides reassurance that their preferences will be respected, even if they are far from home.
Making critical information available where it’s needed most
In Devon and Cornwall, TEPs have been digitised within their shared care record since October 2023 with the ultimate objective being to ensure that everyone involved in a patient’s care, across primary care, hospitals, community services, hospices and ambulance trusts, is working from the same, up-to-date plan.
TEPs are vital forms that are part of the care planning process, supporting the wishes of patients who are unstable or at risk of dying. These plans are captured digitally and held within the DCCR. They help ensure the patient’s treatment goals are clearly developed, understood, and accessible to all members of their care team.
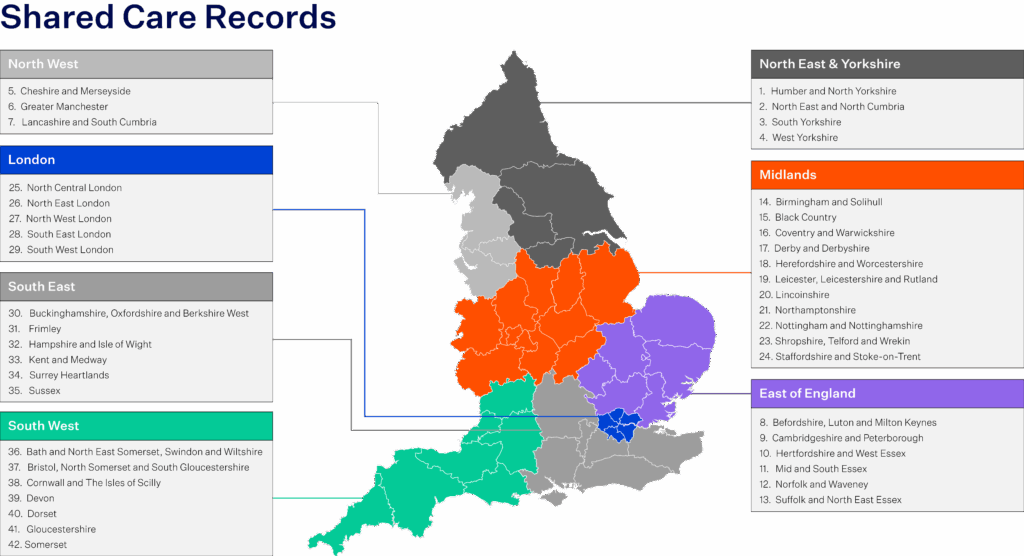
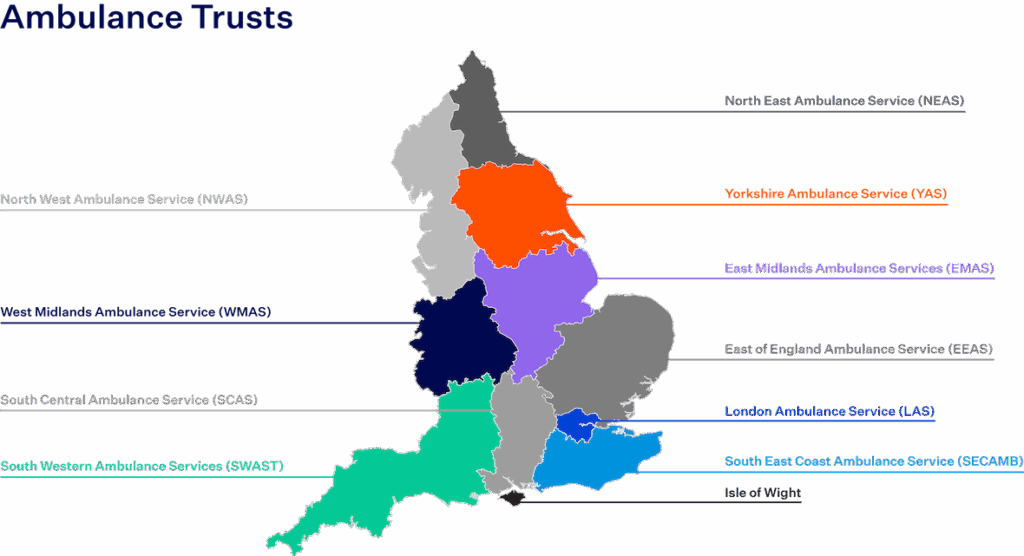
While the digitised TEPs make a huge difference for health and care teams using DCCR, South Western Ambulance Service Trust (SWAST) teams, who provide 999 services across the entire South West, work across multiple ICS boundaries so needed a single point of access to view these critical documents. This is made possible using the National Care Records Service (NCRS).
Connecting TEPs from DCCR to the NRL means they are discoverable to both SWAST paramedics, and six of the other ten ambulance trusts in England also using the NCRS. In addition, SWAST paramedics benefit from having access to digital care plans created elsewhere in the country, which is particularly important for a region like the South West where millions of tourists visit each year. With national access to care plans, paramedics can make confident, informed decisions in emergencies that reflect what matters most to each patient and their family.
“Enabling our paramedics and front line emergency workers to see vital information about a person’s choices for care is a gamechanger for our local population. This development will make sure that people receiving health and social care, especially in urgent and emergency situations, are supported to remain at home and can avoid visits to hospital and possible admissions into secondary care. In Devon and Cornwall we want to provide care in the most appropriate setting for people and often this is in their own home. This technology has provided our system partners to be able to do this with clear clinical guidance which takes into account a person’s choices.”
- Jane Bullard, Clinical Leadership and Partnerships Development Manager, NHS Devon
Delivering the foundations for safer, joined-up care
This was the first deployment of its kind in England to use the NRL’s new FHIR v3.0 API, a modern and scalable standard designed to support faster performance and future growth.
The project was delivered as a collaboration between Orion Health, Devon ICB and NHS England with a shared goal of ensuring high-value clinical documents, such as TEPs, could be made visible and accessible to emergency and urgent care teams across the country, not just within the local system.
The work that supported the go-live included:
- Publishing pointers to the NRL for TEP forms completed in DCCR
- Migrating 27,000 existing TEPs to the NRL, so patients with previously completed forms are now represented nationally in real-time
- Developing a new, scalable NRL integration application to support publication, registration and monitoring of pointers using the v3.0 FHIR API
- Building a secure and governed model for sharing sensitive clinical information with role-based access and audit controls
- Passing a rigorous national accreditation process to ensure compliance with NHS technical and clinical safety standards.
“The ability for our clinicians to check TEP status remotely, in person and in real time is hugely beneficial. It helps us give our patients the right care at the right time in the right place which is our ultimate goal. TEP status is important for guiding decision making and ensuring that our actions are in line with the best interests of our patients. Clarity in difficult situations allows for more dignified care and a better experience for patients and their families in often upsetting circumstances “
- Samuel Taylor, Clinical Lead (South & West Devon), South Western Ambulance Service
Part of a bigger picture: Supporting the priorities of the NHS 10-Year Plan
This deployment is part of a broader journey towards joined-up, person-centred care. Across shared care records, national services and citizen-facing tools, this work contributes to the NHS’s 10-Year Plan vision for a connected health and care system.
The plan highlights ambulance services as integral partners in Integrated Neighbourhood Teams with access to real-time patient information. It describes a future where paramedics responding to a 999 call can instantly see a patient’s care history, allergies and care preferences, reducing duplication and enabling more personalised decisions.
At the heart of this vision is the goal of a Single Patient Record, where a person’s essential health information is in one place and can be accessed wherever they are in the country. Making TEPs visible nationally through the NRL is a key stepping stone towards that goal. It allows critical data to follow the patient across regional and organisational boundaries in real-time, ensuring care is continuous and informed even when people are far from home.
This is one piece in the wider puzzle of national interoperability. It lays important foundations for a future where the right information is available to the right people at the right time, supporting better care for patients and a more connected health service for all.
Quote from OH UK leadership:
“This is just one example of how we’re helping our customers deliver on the priorities of the NHS 10-Year Plan. By focusing on interoperability and open standards, we’re enabling information to move securely across systems and regions. That capability is critical to joining up care, empowering professionals on the frontline and ensuring that vital information follows patients wherever they are, whenever it is needed.”
Looking Ahead
Over the coming months, NRL functionality will be extended to additional Orion Health-powered shared care records in other regions, including publishing nationally recognised ReSPECT forms to the NRL. These forms capture a person’s preferences for emergency care and once connected to the NRL will also become discoverable nationally.
In addition to this, Orion Health is developing capabilities to:
- Generate and share International Patient Summaries (IPS) via the NRL, supporting urgent treatment, cross-border care and safer patient transfers; and
- Retrieve and consume patient records via the NRL, so that Orion Health shared care record users can view documents published by organisations in other regions across England, supporting full two-way interoperability.
These innovations will build on the foundations already in place and bring the NHS closer to a future where vital patient information moves seamlessly across systems and regions.



