Personalised medicine, once aspirational, is now a central force in transforming healthcare. By tailoring interventions to an individual’s genetic, environmental, and lifestyle factors, this approach promises to deliver the right treatment to the right person at the right time.
The rise of precision medicine in clinical care
Thanks to rapid advances in genomics, bioinformatics, and digital health technologies, precision medicine enables clinicians to:
- Predict individual disease risks
- Stratify patient groups for targeted care
- Deliver targeted therapies
Source: Frontiers in Genetics
This timeline highlights key scientific and technological breakthroughs that have enabled the evolution of personalised medicine from theory to practice.
Personalised approaches are already producing tangible results across specialties:
- Genetic screening for BRCA mutations or Lynch syndrome can dramatically reduce cancer morbidity through early intervention.
- In cancer care, personalised medicine has shown the potential to reduce unnecessary treatments and adverse events.
These interventions improve patient outcomes and often reduce long-term healthcare costs, making a strong case for public investment.
Public Health meets personalised medicine.
Traditional public health has long focused on population-wide interventions, such as vaccination, clean water, and anti-smoking campaigns designed for broad populations. Personalised medicine shifts this paradigm, emphasising individual differences over one-size-fits-all strategies.
This shift has led to perceived tensions:
Does focusing on the individual divert resources away from proven, population-wide interventions?
However, recent thinking reframes this tension as an opportunity. Genomic insights can enhance public health surveillance and allow for more efficient, targeted interventions.
From conflict to complementarity
The COVID-19 pandemic demonstrated this convergence. Genomic sequencing allowed for:
- Rapid identification of virus mutations
- Targeted vaccine development strategies
Source: Vicente, Astrid M., Wolfgang Ballensiefen, and Jan-Ingvar Jönsson. “How personalised medicine will transform healthcare by 2030: the ICPerMed vision.” Journal of translational medicine 18 (2020): 1-4.
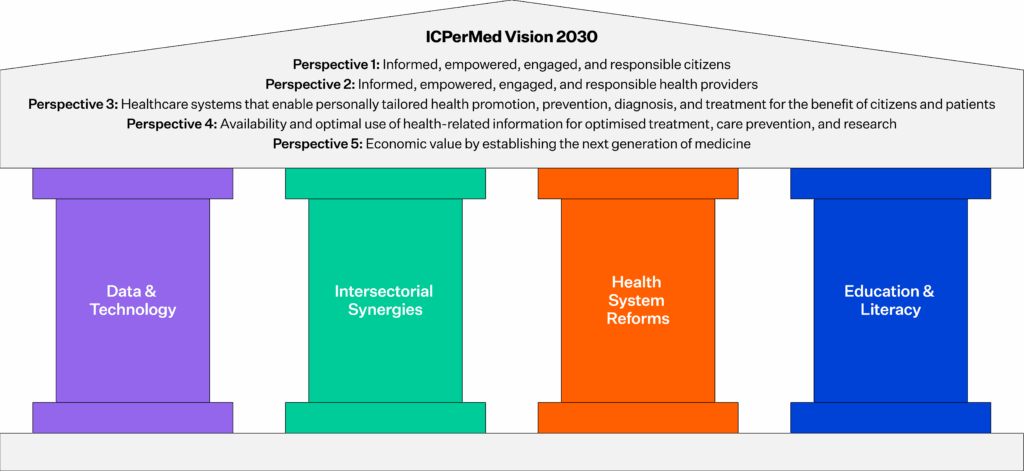
This graphic illustrates the ICPerMed vision for how personalised medicine can enhance healthcare systems by 2030, including its role in prevention, diagnosis, and treatment.
Emerging concepts like “precision public health” seek to bridge the gap by applying the tools of personalised medicine, big data, machine learning, and stratification to optimise interventions across entire populations. The vision is not to abandon broad public health strategies but to refine and personalise them.
Challenges to widespread integration
Despite its potential, personalised medicine still faces barriers to scaling within public health systems:
- Digital infrastructure gaps: Many health systems lack the digital, analytical, and clinical capacity to integrate high-throughput data from genomics, wearables, and EHRs into care pathways.
- Workforce limitations: There is a persistent shortage of skilled professionals able to interpret and apply genomic data, and without multidisciplinary teams and updated clinical guidelines, implementation will remain patchy.
- Equity concerns: Advanced therapies and diagnostics risk widening existing health disparities. If left to market forces, precision medicine may serve primarily affluent populations unless policies ensure broad accessibility.
While personalised approaches can reduce costs related to adverse events and avoidable treatments, initial investments are high. Public systems must carefully assess value and sustainability. Studies show cost savings from reduced adverse events and end-of-life care, but these must be balanced against initial diagnostic and treatment costs.
The future: Hybrid models for sustainable, equitable care
Personalised medicine and public health don’t have to be at odds. The most resilient health systems will be those that:
- Integrate genomics into routine care pathways
- Use risk stratification to drive prevention strategies
- Tailor interventions without sacrificing population-wide equity
To unlock the full value of personalised healthcare, systems need coordinated investment in:
- Interoperable data platforms
- Multidisciplinary workforce development
- Robust governance and ethical frameworks
Serving the public good through personalisation
With the right vision and infrastructure, personalised medicine can do more than treat individuals; it can uplift entire populations. However, without deliberate, inclusive strategies, it risks becoming a tool of privilege rather than progress.
Authored by Tom Varghese, Global Product Marketing & Growth Manager at Orion Health
References
Abrahams, Edward. 2024. “Personalized Medicine: Past, Present, and Future.” Inside Precision Medicine, November 6, 2024. https://www.insideprecisionmedicine.com/topics/precision-medicine/personalized-medicine-past-present-and-future/.
Boccia, Stefania. 2014. “Why Is Personalized Medicine Relevant to Public Health?” European Journal of Public Health 24(3): 349–350. https://doi.org/10.1093/eurpub/cku030.
Cox, David. 2023. “The Quest for the Era of Personalised Medicine.” BBC Future, June 5, 2023. https://www.bbc.com/future/article/20230602-are-we-entering-the-era-of-personalised-medicine.
Cuari, Benedette. 2020. “The Past, Present, and Future of Precision Medicine.” News Medical, February 7, 2020. https://www.news-medical.net/life-sciences/The-Past-Present-and-Future-of-Precision-Medicine.aspx.
EPM Scientific. 2023. “Public Health vs. Personalised Medicine: Bridging the Gap.” EPM Scientific, September 2023. https://www.epmscientific.com/en-au/industry-insights/hiring-advice/public-health-vs-personalised-medicine-bridging-the-gap.
European Federation of Pharmaceutical Industries and Associations (EFPIA). 2023. “Precision Medicine and Population Health: A Contradiction or a Way Forward?” EFPIA Blog, October 4, 2023. https://www.efpia.eu/news-events/the-efpia-view/blog-articles/precision-medicine-and-population-health-a-contradiction-or-a-way-forward/.
Greely, Henry T. 2023. “Public Health versus Personalized Medicine.” Science 381(6659): 738. https://doi.org/10.1126/science.adj0281.
Traversi, Deborah, et al. 2021. “Precision Medicine and Public Health: New Challenges for Effective and Sustainable Health.” Journal of Personalized Medicine 11(2): 135. https://doi.org/10.3390/jpm11020135.
Vicente, Astrid M., Wolfgang Ballensiefen, and Jan-Ingvar Jönsson. 2020. “How Personalised Medicine Will Transform Healthcare by 2030: The ICPerMed Vision.” Journal of Translational Medicine 18: 180. https://doi.org/10.1186/s12967-020-02316-w.




