Reconciling short-term priorities with long-term aspirations is no easy feat, especially in a world where disruption is the norm. From pandemics to global supply chain crises, health systems are constantly tested, revealing deep-rooted vulnerabilities.
But what if health systems could do more than merely survive these shocks?
Enter antifragility, a capability that offers a new blueprint for sustainable, future-ready healthcare.
What Is Antifragility?
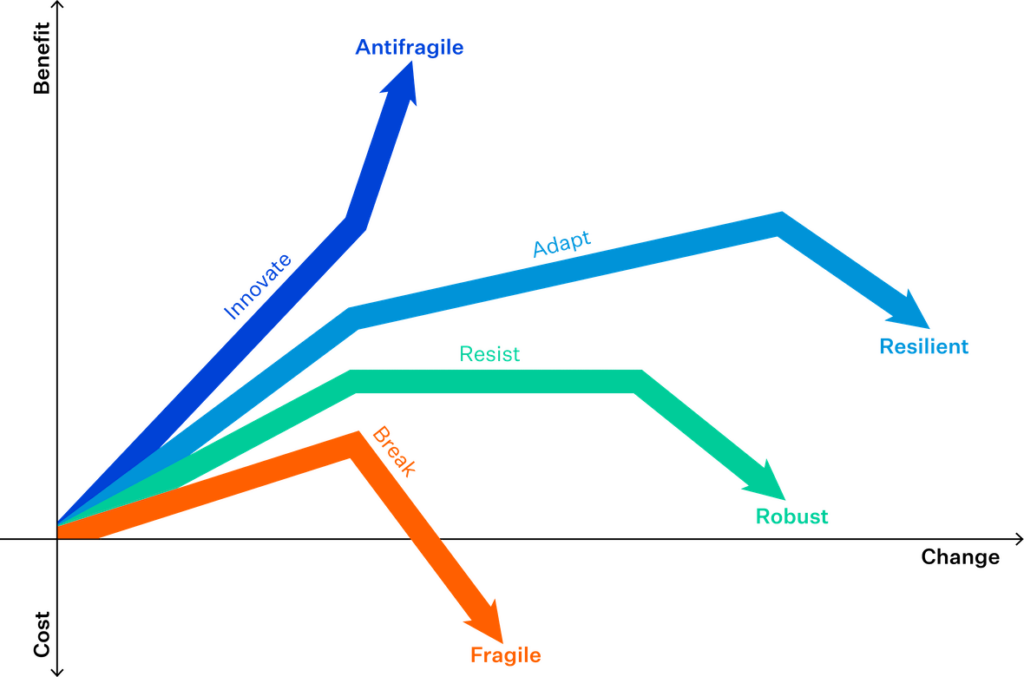
Nassim Nicholas Taleb coined the term antifragility, which describes systems that don’t just resist shocks. They grow stronger from them. Unlike resilience, which is about bouncing back, antifragility is about bouncing forward.
In healthcare, this mindset reframes volatility as an opportunity to evolve, rather than a threat to stability.
The three core strategies for antifragile health systems
To move from reactive to antifragile, health systems must embrace three strategic shifts:
1. Embracing Optionality
Health systems with multiple care delivery modes, such as in-person consultations, telehealth, and mobile care, are better equipped to adapt during disruptions. Optionality enables rapid pivots when traditional care settings are compromised.
During the COVID-19 pandemic, decentralised models proved essential, helping providers seamlessly switch between care modes.
Source: Critical Care Now
2. Leveraging hybrid leadership: Balancing strategy and autonomy
In times of uncertainty, the most effective responses arise from distributed leadership. This means empowering frontline workers to act independently, while aligning their actions with a clear strategic vision from the top.
Organisations with strong, distributed leadership respond quickly and innovatively to local needs, turning frontline insights into systemic improvements.
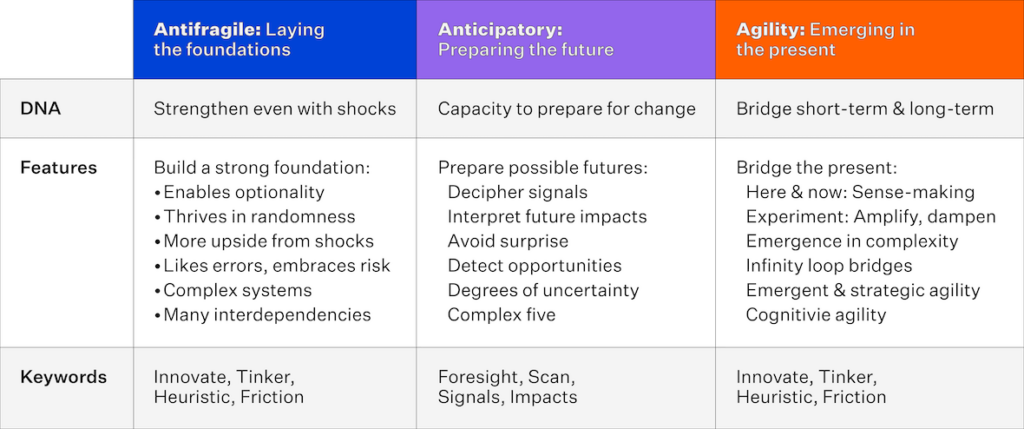
AAA Framework for Anticipatory Governance
Source: World Economic Forum
3. Adopting iterative learning and nonlinear evaluation
Antifragile systems don’t wait for perfection—they act, learn, and iterate. Small-scale tests, frequent feedback loops, and learning from failure allow organisations to adapt quickly and improve continuously.
This agile mindset allows health systems to adapt, rapidly scaling successful interventions and abandoning ineffective ones without excessive loss.
The role of digital infrastructure in antifragility
Digital transformation underpins all three strategies. Cloud-based systems, real-time data access, and interoperable platforms allow for:
- Faster response to emerging needs
- Scalable and adaptable care delivery
- Better coordination across diverse care settings
Tech companies like Amazon exemplify antifragility through digitally enabled, decentralised systems that continuously evolve from disruptions.
Health systems can take a page from this playbook, leveraging technology not just for efficiency, but for adaptability.
Real-world examples of antifragility in healthcare
New Zealand
New Zealand’s GPs demonstrate antifragility by serving as the cornerstone of care, delivering over 21 million patient visits annually, far outpacing emergency department visits.
This decentralised model proved resilient and responsive during the pandemic, keeping patients connected to primary care even as hospitals faced strain.

Source: The New Zealand Initiative
England
Integrated Care Systems (ICS) in England reflect antifragile design by bringing together providers, payers, and communities. This model allows them to coordinate care, respond dynamically to local needs, and evolve based on real-time learning.
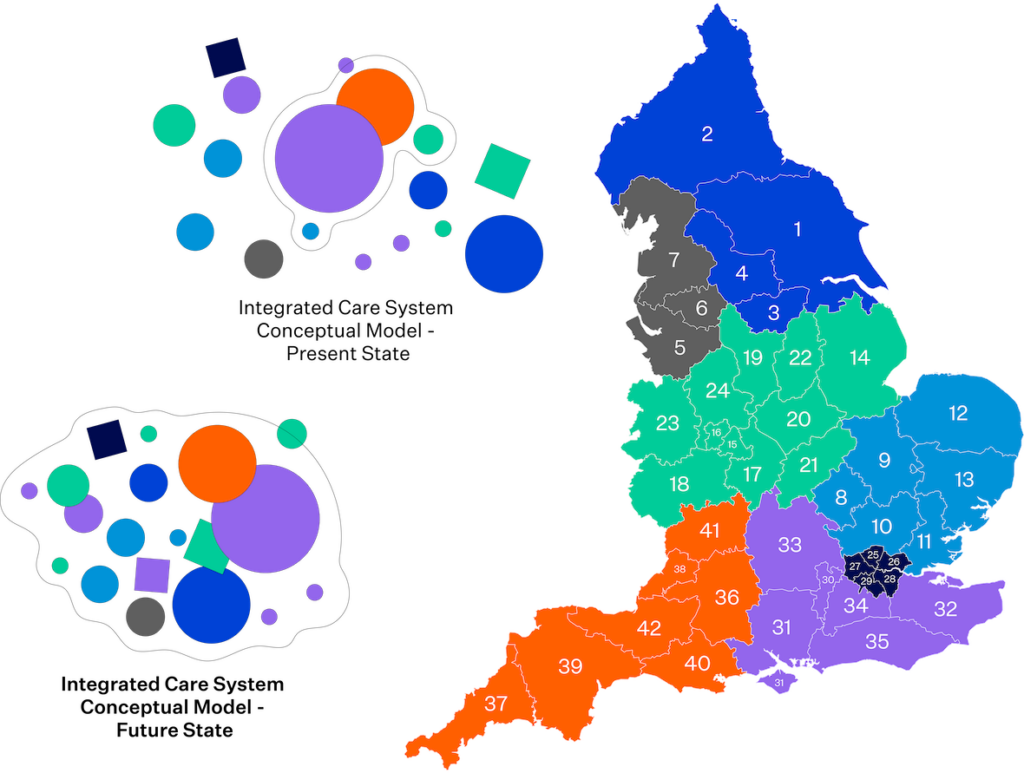
Source: Mid and South Essex Integrated Care Strategy 2023-2033
From Fragile to Future-Ready
Health leaders, policymakers, and clinicians must hardwire antifragility into their organisations. Health leaders, policymakers, and clinicians must embed antifragility into their organisational DNA. Prioritising optionality, hybrid leadership, iterative learning, and digital transformation creates systems that do not just recover but actively improve from stressors.
Ultimately, an antifragile health system treats each disruption as a chance to innovate and strengthen. It is not about merely weathering storms; it’s about harnessing their energy for meaningful, lasting improvement.
Disruption is inevitable. But how we respond to it will determine the future of healthcare.
References:
- Al-Azri, Nasser Hammad. “Antifragility Amid the COVID-19 Crisis: Making Healthcare Systems Thrive Through Generic Organisational Skills.” Sultan Qaboos University Medical Journal 20, no. 3 (2020): e241–e244.
- Botjes, Edzo, Martin van den Berg, Bas van Gils, and Hans Mulder. “Attributes Relevant to Antifragile Organizations.” In 2021 IEEE 23rd Conference on Business Informatics (CBI). IEEE, 2021.
- Joarder, Amitabha (Jordy). “Antifragility and the Journey of Organisations on Being Antifragile.” LinkedIn, June 2, 2020.
- Murray, Bill. “Building an Antifragile Organisation.” CEO Today, October 21, 2020.
- Petrie, Samuel, and Paul Peters. “Health Service Implementation and Antifragile Characteristics in Rural Communities: A Dirt Research Approach.” International Journal of Environmental Research and Public Health 20, no. 14 (2023): 6418.
- Rebhan, Andrew. “A Lesson in Antifragility for Digital Health Startups.” LinkedIn, August 31, 2022.
- Sahdev, Navroop, Gurvinder Ahluwalia, and Mike Durrie. “The Antifragility Effect: Deploying Emerging Tech in Medical Device Supply Networks to Rebuild Better.” SSRN, 2021.
- Zahid, Bassam. “2021: The Year of the Antifragile Resuscitationist.” CriticalCareNow, January 1, 2021.




