Public health systems worldwide are at a tipping point. Should we continue operating within outdated political and policy structures or take bold steps toward building resilient, forward-thinking systems?
The recent announcement to abolish NHS England (NHSE) provides a powerful case study of the risks and realities of large-scale healthcare reform. While the NHS has long been admired as a model of universal healthcare, its recent struggles highlight the dangers of chronic underfunding, political interference, and reactive policymaking.
NHS: A Decade of Underinvestment and Mounting Pressure
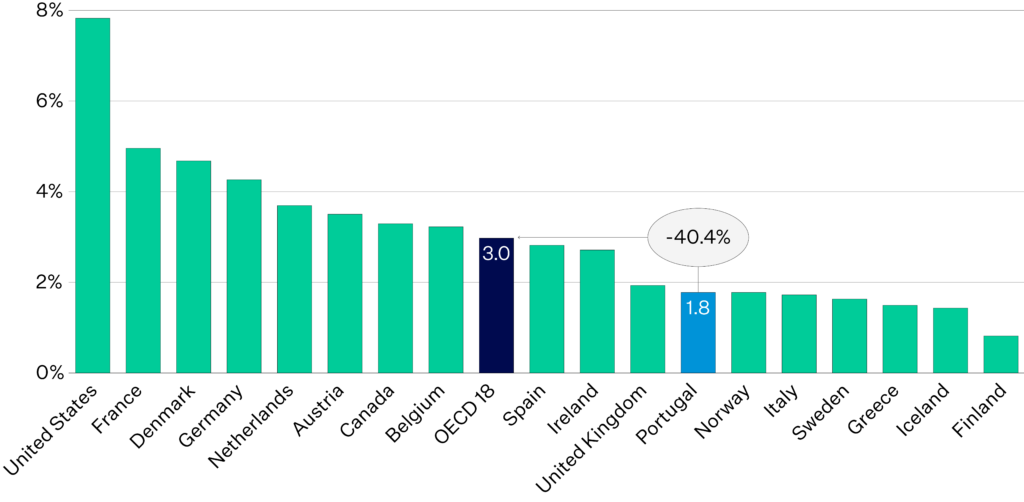
Between 2010 and 2020, NHS funding grew by just 1% per year in real terms, well below the historical average of 3.4% annually. This underinvestment, combined with an ageing population and rising healthcare costs, led to increased waiting times, overwhelmed services, and falling public satisfaction.
Source: https://www.theguardian.com/society/2025/mar/14/what-were-the-lansley-reforms-and-how-did-they-create-nhs-england
Despite its enduring reputation, the NHS has struggled to meet growing demand under financial constraints.
Abolishing NHSE: Reform or Risk?
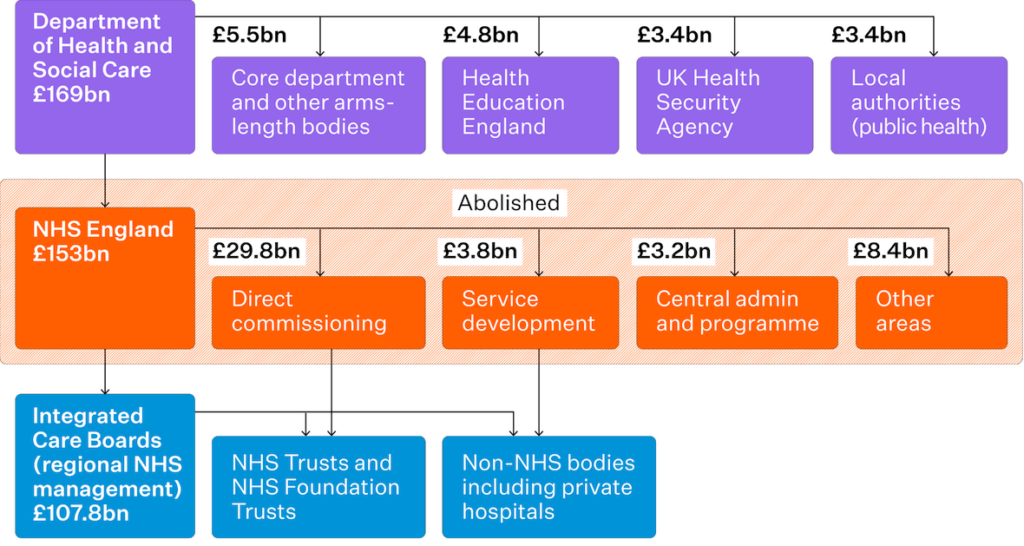
The UK Government’s decision to dissolve NHS England was framed as a move to streamline decision-making and bring health services back under democratic control. Its functions are set to be redistributed across the Department of Health and Social Care and regional Integrated Care Boards (ICBs).
But will this change deliver genuine improvement—or add more layers of complexity?
NHSE was created in 2012 as an independent statutory body designed to depoliticise healthcare management and oversee funding allocations. Over time, however, political interference eroded its autonomy. This tension between centralised oversight and regional authority continues to challenge health system reform.
The Cost of Constant Restructuring
Structural reform is often promoted as a cost-saving measure, but the reality is more complex. The abolition of NHSE is expected to result in significant redundancy costs and consultancy fees, potentially diverting funds from frontline services.
Constant reorganisation also disrupts leadership continuity and workforce morale—two key ingredients for long-term system resilience. Without strategic oversight, cost-cutting can exacerbate inefficiencies rather than resolve them.
Source: Independent Investigation of the National Health Service in England – The Rt Hon. Professor the Lord Darzi of Denham OM KBE FRS FMedSci HonFREng
Public Health Needs a Shift in Focus
From 2016 to 2022, the local authority’s public health grant fell by 21% in real terms. This decline underlines a broader trend: reactive, hospital-based care continues to be prioritised over preventative and community-driven healthcare.
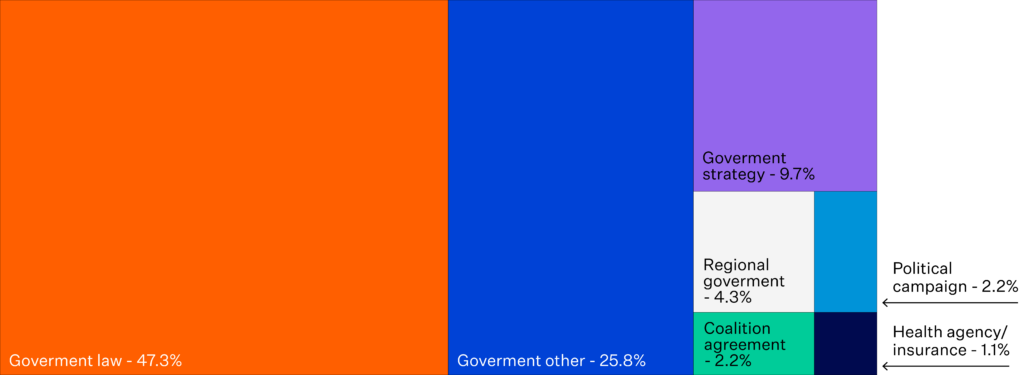
Source: “Top-Three” health reforms in 31 high-income countries in 2018 and 2019: an expert informed overview
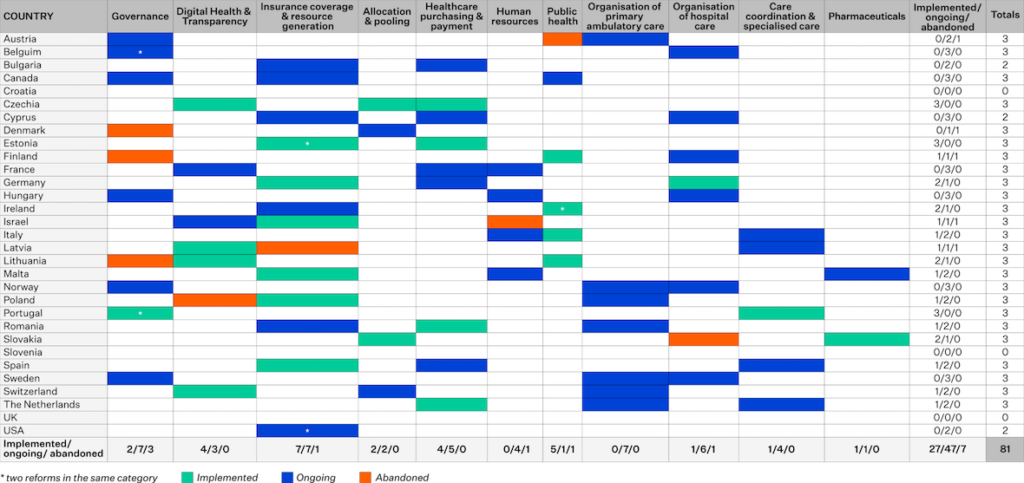
Implementation Status of Health System and Policy Reforms Across High-Income Countries, 2019
Source: “Top-Three” health reforms in 31 high-income countries in 2018 and 2019: an expert informed overview
Evidence shows that investing in upstream interventions—such as community services, health promotion, and tackling social determinants—delivers tangible outcomes and improves long-term system sustainability.
Rethinking Reform: What Global Health Systems Can Learn
Health systems around the world can draw key lessons from the NHS experience:
- Focus on long-term resilience: Investment in digital transformation, infrastructure, and the workforce is crucial to improving efficiency and outcomes.
- Balance local autonomy with national accountability: Empower regional authorities but maintain national oversight through transparent performance metrics.
- Invest in prevention: Published evidence shows that addressing social determinants of health through targeted interventions and increased funding for community healthcare has tangible outcomes.
Choose Stability Over Short-Termism
The NHS serves as a cautionary tale of a well-intentioned but mismanaged system. It’s a clear reminder: Future health systems must avoid the pitfalls of short term political interventions and instead focus on long term resilience, sustainable funding, and patient centred care.
The choice is clear. Perpetuate a cycle of instability or build a robust, adaptable system that genuinely serves public health needs.
Discover how Orion Health’s Shared Care Records enable connected, patient-centred care across health and care systems.