Digital health is evolving rapidly, but despite innovations in AI, data platforms, and diagnostics, many solutions fail to take root. Why? Because too often, they are built around technology, not people.
To make a meaningful impact, health tech must do more than showcase digital sophistication. It must solve real problems for real people, clinicians, patients, and administrators within the messy, complex environments where care is delivered. Success depends on understanding context, behaviour, and trust.
Understand the problem before building the product.
Empathy is the foundation of effective digital health innovation. Instead of jumping into technical solutions, successful innovators start by deeply engaging with the problem.
This means asking:
- What exactly needs fixing?
- Who is affected and how?
- What does this challenge look like in day-to-day practice?
Crucially, this user research must include voices from across the healthcare spectrum: doctors, nurses, patients, administrative staff, and IT support. By mapping the whole picture, teams can avoid designing for hypothetical workflows and ground solutions in reality instead.
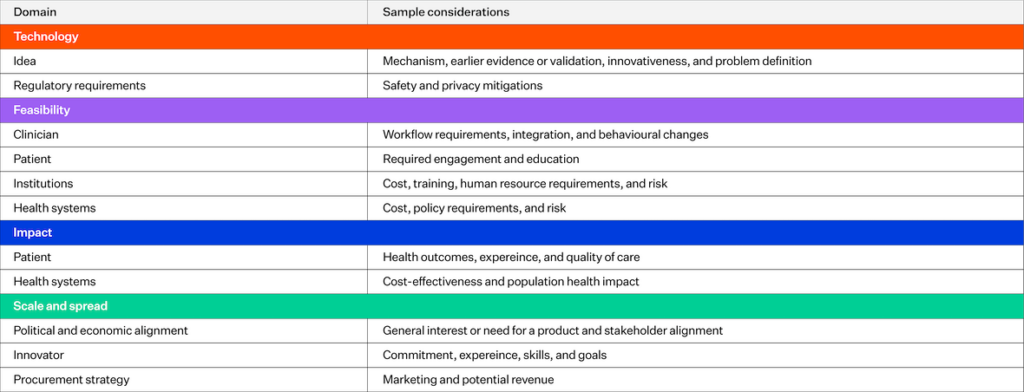
Source: Kelley, Leah Taylor, Jamie Fujioka, Kyle Liang, Madeline Cooper, Trevor Jamieson, and Laura Desveaux. “Barriers to creating scalable business models for digital health innovation in public systems: qualitative case study.” JMIR public health and surveillance 6, no. 4 (2020): e20579.
This framework highlights the range of interdependent factors that can make or break a digital health product. It reinforces the need to consider clinical value, usability, and business viability early on.
Align with the needs of every user group.
Healthcare is never a single-user environment. A tool designed to streamline nurse workflows may inadvertently increase doctors’ admin time. A digital platform meant to empower patients may confuse older users or overwhelm caregivers.
That’s why a successful solution must align with the needs, values, and constraints of every group involved. This includes understanding:
- How each role defines value
- How workflows intersect or clash
- What unintended burdens might arise
Tailoring digital solutions to accommodate the full ecosystem of users creates a smoother path to adoption and long-term sustainability.
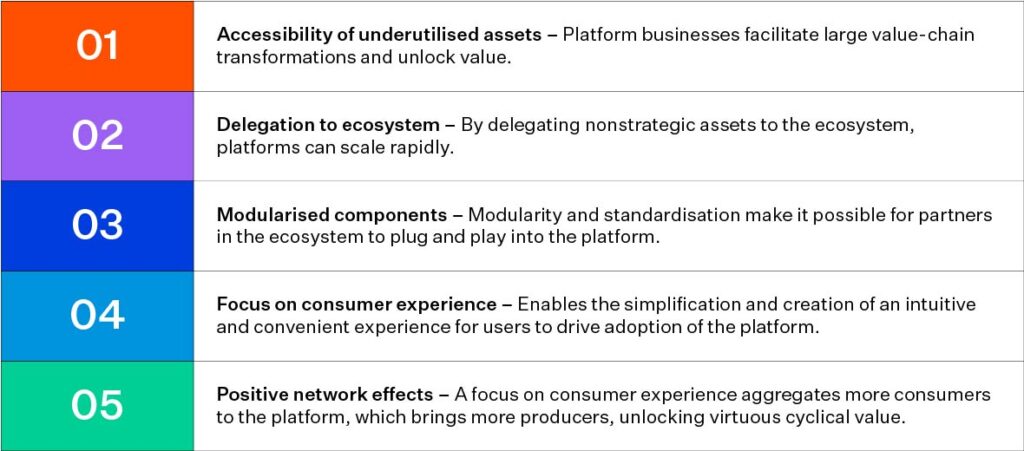
Source: Deloitte Health Care Ecosystem
This visual illustrates how digital health platforms must embed themselves into broader health system structures to generate lasting value.
Build trust through co-creation
In healthcare, trust is just as critical as functionality. Asking clinicians or patients to change how they work or manage their care requires a compelling reason. One of the best ways to foster trust is through co-creation.
By involving users from the outset and iterating based on their feedback, companies can:
- Adapt to real-world use
- Improve usability and relevance
- Cultivate user ownership and buy-in
When people feel heard and involved, they’re more likely to support, champion, and stick with a new solution.
Respect structural and financial realities
Even the most elegant digital tool can fail if it doesn’t fit the system it enters. Procurement rules, funding structures, and legacy IT can all become roadblocks.
Digital health innovators must understand:
- What budget cycles and purchasing constraints look like
- How interoperability fits into existing infrastructure
- Whether the solution is feasible for system-wide rollout
Being realistic about what health systems can absorb and building accordingly makes innovation viable, not just visionary.
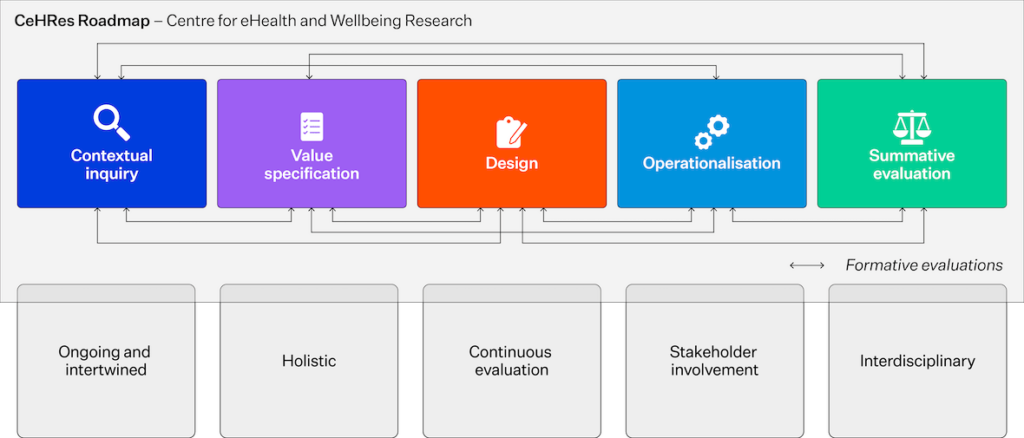
Source: CeHRes: Centre for eHealth and Wellbeing Research
The CeHRes Roadmap is a structured framework developed in the Netherlands to guide the development, implementation, and evaluation of eHealth technologies. It is widely used in digital health projects to ensure that technological innovations are not only effective but also usable, desirable, and sustainable within real-world healthcare settings.
This framework guides the development, implementation, and evaluation of digital health technologies with a strong focus on real-world fit and iterative learning.
Define outcomes that matter.
Funders, users, and health leaders all want to know: How will this improve care?
Articulating clear, measurable benefits is key. Whether it’s:
- Fewer hospital visits
- Shorter appointment times
- Less paperwork
- Improved patient wellbeing
These outcomes give stakeholders a reason to embrace change. When shared transparently, the benefits create a ripple effect of trust, adoption, and advocacy.
People-led tech is the future of health.
The most successful health tech solutions are designed with users, not just for them. This requires a shift from technology-first to people-first thinking; listening deeply, adapting quickly, and valuing real-world impact over digital novelty.
By embedding these principles into every stage of innovation, we can ensure that digital tools fit naturally into care, not as burdens, but as trusted allies in better health outcomes.




