Without any warning, a member of your family could become a victim of stroke. Will you be prepared? Who will look after them? How long will they need care for and how dependent will they be? Can you take time off work to look after them or do you need to arrange other care?
One of the biggest struggles of being a patient is not knowing what your body is going to do. When a serious health event does happen, it can be particularly disturbing for a patient and their family especially if it has a long-term impact. By offering patients legitimate expectations for recovery time and level of dependency, it reduces the worry of uncertainty on patients and their families.
Precision Driven Health (PDH), a public-private research partnership between Orion Health, Waitemata DHB and the University of Auckland, has recently developed a tool that uses machine learning to predict stroke outcomes.
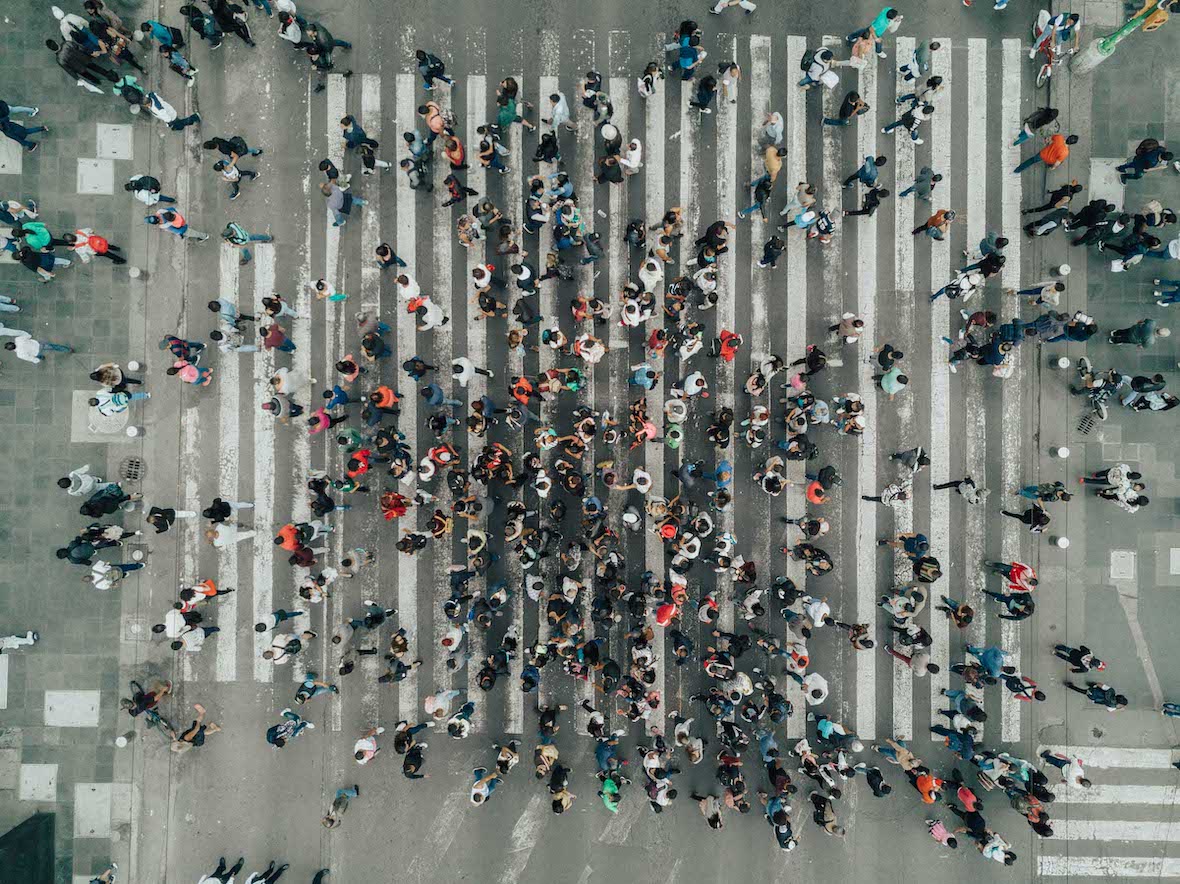
Stroke is the major cause of serious adult disability in New Zealand and kills around 2,500 people every year1. For the approximately 60,000 stroke survivors and their families in New Zealand, stroke has been a devastating life-changing event causing disabilities such as partial paralysis – which leads to survivors, often elderly, having to learn to walk and talk again.
Recovery can vary significantly, and it is especially hard for patients and clinicians to plan for it without knowing the outcome of the stroke. The HOPE (Health Outcome Prediction Engine) for Stroke project aims to tailor care to stroke patients, providing them with as much information or preparation that is available, to help manage their own and their families’ expectations.
The HOPE for Stroke project lead by Waitemata DHB’s Peter Sandiford, falls under PDH’s predictive analytics theme, the purpose being to demonstrate how machine learning can help patients and clinicians prepare for health outcomes. In this case, the tool is designed to predict stroke recovery, giving patients and their families the opportunity to adjust their expectations and work with care providers to prepare for recovery.
The system uses data from the Waitemata DHB Stroke Register to examine 2800 strokes over the past five years. It analyses existing socio-demographic and clinical variables such as stroke severity, living conditions, age, time spent in ED, and uses these to predict outcomes following the stroke such as length of stay and rehab requirements.
When clinicians are in the stroke assessment system, they are asked to make their own prediction of what they think is most likely to happen to the patient. The system saves the prediction, as well as the engine’s prediction of outcomes including level of dependency, and records what the outcome actually was one month after the stroke.
The innovative new tool is ready to be tested with stroke patients, as the machine learning predictions have proven to be very accurate. The next stage is for clinicians to find the most useful way to use this tool in their systems.