In the evolving world of healthtech, a persistent gap remains between an organisation’s willingness to buy and its willingness to pay. While many healthcare stakeholders express enthusiasm for adopting digital innovations, budget realities often tell a different story. This tension raises a critical question: What truly defines value in health technology today?
Understanding the healthtech buyer collective
A single decision-maker no longer defines today’s health tech purchasing landscape. Instead, a “buyer collective,” including clinical leads, IT experts, finance officers, and operational managers, evaluates and approves investments. Their shared challenge? Balancing clinical impact with fiscal feasibility.
Decision-making cycles now often stretch over 18 months, reflecting not just bureaucracy but deeply entrenched systemic constraints.
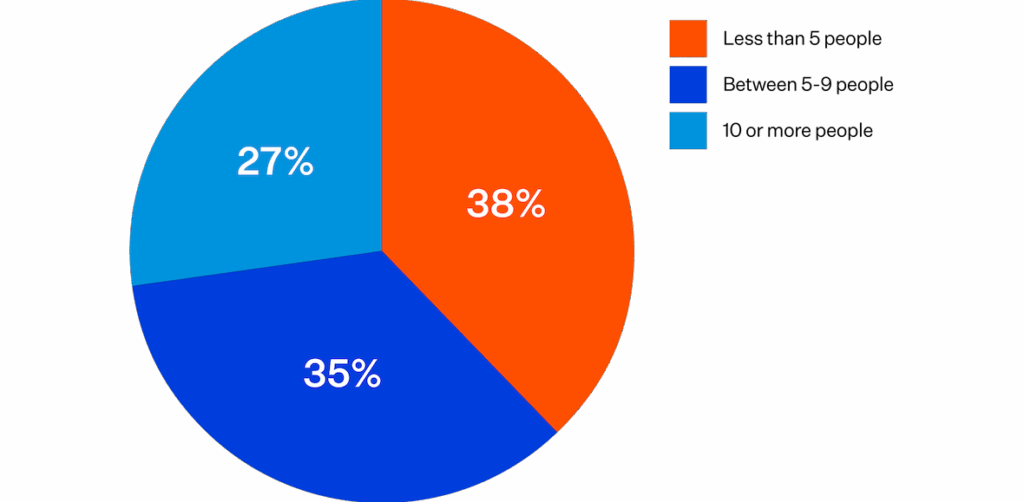
Source: 2024 HIT Buyer’s Survey of HIMSS Enterprise Audience; N=86
These prolonged cycles are shaped by factors such as:
- Annual budgeting frameworks
- Regulatory oversight
- A prioritisation of short-term affordability over long-term transformation
Even when solutions offer clear benefits, they must pass through a labyrinth of procurement processes and compliance checks before being seriously considered.
Willingness to buy: High interest, high complexity
Digital transformation is not a hard sell. Healthcare organisations are actively exploring innovations from AI-powered diagnostics to integrated electronic health records. Over 80% of buyers now initiate vendor contact themselves, often reaching advanced stages of consideration before formal engagement begins.
Source: Gartner
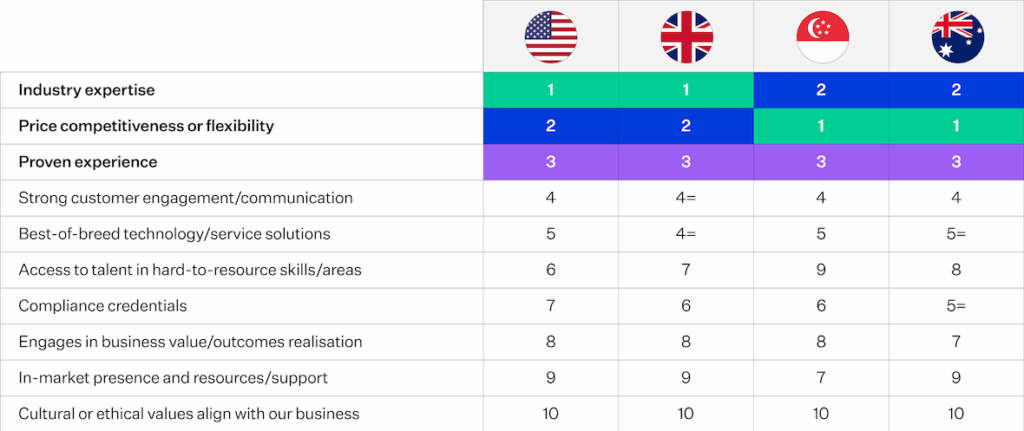
This self-guided behaviour underscores a strong willingness to buy, but it’s highly dependent on:
- Internal research and alignment
- Peer validation and case studies
- Timing within budgeting cycles
The rise of account-based marketing and content personalisation directly responds to these shifts. Buyers want educational content, demos, and clear ROI stories, often long before they’re ready to spend.
Source: NZTE
Willingness to pay: Reality bites
While intent may be strong, willingness to pay is ultimately limited by what a healthcare system can afford. Even the most compelling cost-effectiveness analyses often fail to sway purchasing decisions. Why?
Because:
- Financial benefits may fall outside the current fiscal year.
- Budget holders are now incentivised to contain costs rather than invest in long-term efficiencies.
- Procurement teams tend to focus on technical specifications and upfront costs, not lifetime value or population health outcomes.
As a result, high-impact innovations are often admired but not adopted.
Rethinking value in healthtech
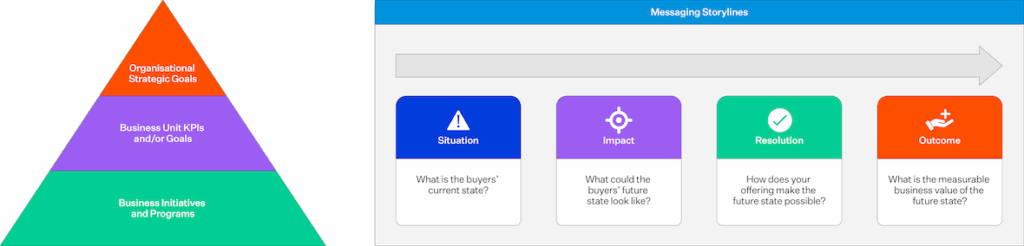
To bridge this gap, vendors must reframe how they articulate value, moving beyond clinical outcomes to showcase:
- Budget-aligned impact
- Workflow integration
- Procurement-readiness
It’s not enough to promise transformation. Vendors must equip internal champions with:
- ROI calculators and business cases
- Regulatory documentation
- Scalable implementation plans
By addressing these practical realities, innovators can shift from being “nice to have” to “ready to deploy.”
Closing the loop between aspiration and adoption
Ultimately, value in healthtech is not just defined by the solution’s potential—its adoptability defines it within a complex, risk-averse system.
To close the gap between willingness to buy and willingness to pay, vendors must align with their buyers’ financial, operational, and cultural realities. This means embedding value narratives into every stage of the buying journey, from early awareness to procurement approval.




