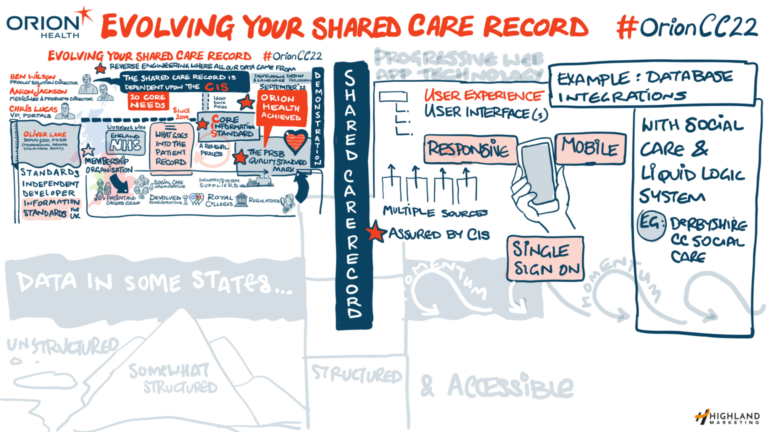
The Orion Health UK and Ireland Customer Conference 2022 is taking place in Bristol. Its theme is how to build on the basic shared care records in place in England in order to make healthcare more efficient for organisations and clinicians, to coordinate care for patients, and to move towards population health management approaches. So, one of the big sessions of the morning was “evolving your shared care record.”
Big news about a big standard
Oliver Lake, deputy chief executive, the Professional Record Standards Body, opened the session by explaining its role. The PRSB is an independent, not for profit, membership body that is responsible for developing standards for UK healthcare, maintaining them, and encouraging their use. With the support of a four-year contract from NHS England, it is PRSB standards that increasingly define the content of healthcare records in the UK.
Oliver told the conference that there are 20 standards in place at the moment, of which the biggest and most important to shared care records is the Core Information Standard, which defines the information that can potentially be shared between systems at different sites and between the professionals using them. The process for deciding whether a supplier has conformed with the standard is “tough.” In fact, it’s so tough that only one supplier has passed the conformance process – Orion Health.
“This happened just this week, and it is a landmark process for us,” Oliver said. “There are more than 1,600 items in the standard and it has taken more than 20 meetings between Orion Health and ourselves to achieve this. It has been a really collaborative process, and now we want this to be an industry movement. We want people to see this as the start of a movement towards everybody thinking about how to implement standards in their systems correctly.”
Rethinking shared care record design principles
Ben Wilson, product solution director, Orion Health, said it had taken a year to reach this milestone. “At some points, it felt like I was working for the PRSB, we spent so much time on it,” he joked. “Some of the standard was very familiar, but some took a lot of work.” The work was worth it, he said, because it needs to be easier for organisations and their IT systems to share information, and for clinicians and patients to be able to find what they need, safely and easily. “It is the national dataset that all shared care records should adopt.”
Orion Health has also been doing a lot of work on the design of its shared care record, with a view to creating a consistent design framework for use in different use cases. “What is fascinating about designing a shared care record is how you pull all this information together and present it in a meaningful way,” Ben said. “We have come up with the idea of making sure that the most important information is presented first, with an option to drill down for more, and making sure it is really clear what the user is looking at and not looking at.”
So, he said, clinicians now see data in ‘comfortable view’ by default. This shows the provenance of all the data in the record, but users can expand or contract data, to see the information they need at a glance, or find more detail. Some key data, such as safeguarding information, or emergency admissions, has been badged and colour coded, to give users a better story about the patient in front of them.
At the same time, Ben said, Orion Health is determined to introduce more personalisation. The system will ‘remember’ whether clinicians use the comfortable, contracted or expanded data view, and open with those settings the next time they use the record. While changes have been made to the document tree, to make it easier for users to find documents, and to surface the documents they use most the next time they login.
Orion Health has also adopted progressive web app technology, so the shared care record can size for use on a computer or laptop, a mobile, or even smaller devices. While another area of focus has been building integrations with GP, hospital, community and mental health systems; and some specialist systems such as BadgerNet Maternity Notes. “We think this is quite important, because it really encourages adoption of the shared care record,” Ben said. “If there are any other systems out there that you think we should be integrating with, we are really keen to hear about that.”
Social care systems are likely to be top of many shared care record system lists, and Ben said Orion Health has been going through the LiquidLogic system that is used by many local authorities for social care and child protection to work out what is recorded and how it can be included within a shared care record, “of course taking account of the security and sensitivity concerns around that.”
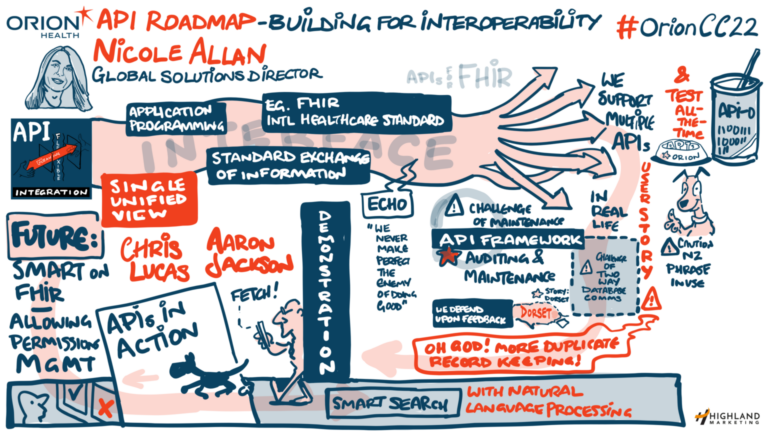
Opening up on APIs
Nicole Allan, global solutions director, Orion Health addressed one of the technical issues involved in creating shared care records, by talking about the role of application programming interfaces, or APIs. Orion Health has a suite of APIs that use international standards, such as FHIR, to make sure that data is shared safely and consistently. When plugged into Amadeus, these make it – relatively! – simple to integrate data from different systems.
Orion Health also has an API framework and list of adaptors or standardised data providers, who can – relatively! – easily share data through APIs. There are challenges. One is that FHIR comes in many versions or flavours “so it is hard even for vendors like ourselves to keep up with them.” So, “behind the scenes” Orion Health has decided to “eat its own dogfood” and to check that its own APIs work by using them for its own portal.
Meanwhile, Orion Health has split the API framework into levels, which focus on issues like security and authentication – and how these are audited. For example, she said two Orion Health users, The Dorset Care Record and the Care and Health Information Exchange in Hampshire, are looking to exchange data within the Wessex Local Health and Care Record Exemplar. They are looking to use the API framework to support this; but they have found that they authenticate data providers in different ways. In future, the framework will make sure that both have full access to authentication information.
Despite this kind of technicality, Alan stressed that the whole point of APIs and standards like FHIR is to make it easier for shared care records to ‘plug and play’ new data feeds and to create a single, unified view for a user or clinician. So, although some early shared care records, like Connecting Care, had to do a lot of work in their early years to get point to point integrations in place, newer Orion Health customers should have a set of APIs, and a list of adaptors available to them “out of the box.”
Eating the dog food – or APIs in action
Aaron Jackson, product director, Orion Health, gave some concrete examples. He started with a view of unstructured data and then gave an example of a consolidated view – Medications Viewer. “Medications information is complex,” he said; it comes from a lot of places – from GPs, hospitals and pharmacies – but standards like FHIR “allow us to bring it all together.”
In England, this can be made available to GPs using the GP Connect standard, while in Scotland it can be mediated through the API framework into GP systems. Another viewer that uses FHIR adaptors is the Immunisation Viewer that was developed at speed for Scotland during the Covid-19 pandemic, and that has now been retained to record and display immunisation information across the country. Jackson said Orion Health is making “a big investment” in the structured data required to develop similar viewers in the future.
Chris Lucas, vice president, clinical portals, Orion Health, rounded out the session by outlining even more developments coming in the future. “Nicole talked about APIs, and it is quite dry, but we have been developing something called SMART on FHIR,” he said. “This enables a third party app to call data from the data platform, using those APIs. “That might also sound quite dry, but if you think about a clinician carrying out a symptom assessment with an online tool such as Ada’s symptom checker, we are able to pass along all of the information from the data platform so the clinician can focus on answering questions, instead of working with the information that the platform has.
“Another great example of this is Boston Children’s Hospital growth chart app, which visualises a growth chart for a child, out of our observations FHIR APIs. The big picture is it means that people can look to build their own applications without worrying about integration between application A and application B.” Chris said there would also be developments in personalisation. For example, he said Orion Health is working on enabling clinicians to personalise their own views of data “so they can do that without a developer being involved.”
Smart search: not just a great idea, but ready to pilot
And, he said, “I am really excited about the Smart Search project” that had already been referred to by Southern Cross Healthcare. Smart Search aims to solve the problem of clinicians going into the shared care record and the document tree, conducting a search, skimming a document, and doing it again. “We are looking to use natural language processing capabilities to search the record and to pull information out of it in a much more natural way,” Chris said.
This is hard, because the system will need to be able to ‘understand’ that terms such as ‘heart attack’ and ‘MI’ are the same thing; and to know that ‘no history of heart disease’ is not a data item that should be returned to a clinician looking for the causes of a patient’s heart disease. Nevertheless, he said, a pilot product is in place at Southern Cross Healthcare – and will be available for delegates to the conference to see tomorrow.



