Health system integration is a complex and multifaceted process that requires the collaboration of multiple stakeholders, including policymakers, healthcare providers, technology vendors, and patients. Achieving a well integrated health platform is not just about technology, it demands strategic alignment, governance, and a patient centred approach.
Key Challenges in Health System Integration
Many healthcare systems continue to operate in silos, with fragmented data spread across hospitals, primary care, specialist clinics, and community services. This fragmentation results in inconsistent care experiences and inefficiencies.
Diverse interests among government agencies, technology vendors, and frontline clinicians further complicate integration efforts. Each group brings different priorities to the table, which can slow progress and dilute impact.
Additionally, robust data governance is essential. Health data is sensitive, and any integration effort must address:
- Data security
- Regulatory compliance
- Patient consent
On top of that, sustained financial investment is required—not just to get systems off the ground, but to ensure they are maintained, upgraded, and adapted as needs evolve.
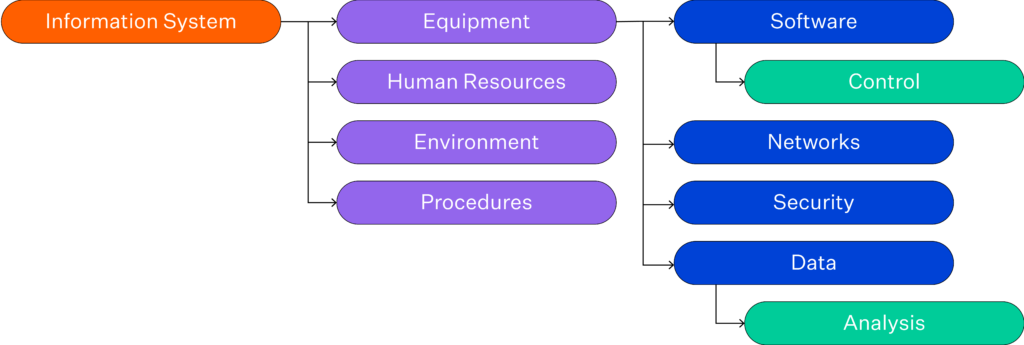
Source: Ștefan, A. M., Rusu, N. R., Ovreiu, E., & Ciuc, M. (2024). Empowering Healthcare: A Comprehensive Guide to Implementing a Robust Medical Information System—Components, Benefits, Objectives, Evaluation Criteria, and Seamless Deployment Strategies. Applied System Innovation, 7(3), 51.
This visual provides a helpful overview of the essential components needed to power an integrated medical information system, from hardware infrastructure to user interfaces and analytics.
Building Blocks for Successful Health System Integration
So, how do we overcome these barriers and achieve a truly integrated platform? It starts with structure.
1. Establish Strong Governance
A clearly defined governance framework is essential. This includes setting roles and responsibilities, developing accountability mechanisms, and fostering a culture of shared ownership across organisations and sectors.
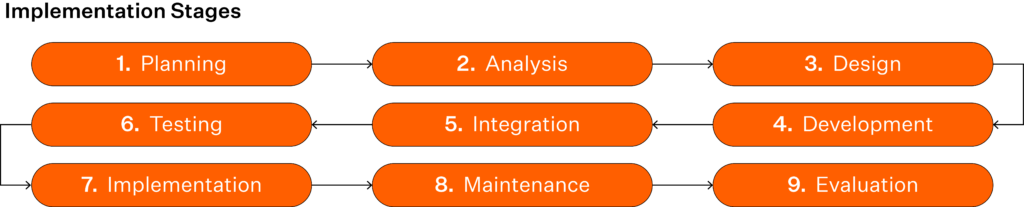
Source: Source: Ștefan, A. M., Rusu, N. R., Ovreiu, E., & Ciuc, M. (2024). Empowering Healthcare: A Comprehensive Guide to Implementing a Robust Medical Information System—Components, Benefits, Objectives, Evaluation Criteria, and Seamless Deployment Strategies. Applied System Innovation, 7(3), 51.
Understanding the staged approach to implementation can help health leaders plan strategically and mitigate risks during roll-out.
2. Prioritise Interoperability Standards
Interoperability must be baked into the foundation of any integrated system. By aligning with global standards like HL7 FHIR, health platforms can support seamless, secure data exchange between providers, settings, and systems.
Learn more about HL7 in Healthcare here.
3. Co-Design with End Users
Engagement is critical. Co-designing solutions with clinicians, administrators, and patients ensures that digital tools reflect real-world workflows and needs—improving adoption and long-term success.

Approaches to digital health tool selection and important considerations for each approach.
Source: Marwaha, J. S., Landman, A. B., Brat, G. A., Dunn, T., & Gordon, W. J. (2022). Deploying digital health tools within large, complex health systems: key considerations for adoption and implementation. NPJ digital medicine, 5(1), 13.
This graph breaks down the key factors health systems should consider when selecting digital tools, from usability to scalability and integration potential.
4. Secure Long-Term Funding
Integration isn’t a one-time project—it’s a continual process of optimisation and evolution. Funding models must reflect that, ensuring there’s capacity to support system upgrades, innovation, and workforce training over time.
Keep the Patient at the Centre
Technology alone won’t transform care. Integration’s ultimate goal is to support care coordination, enable personalised care plans, and provide patients and providers with seamless access to health information. Everything—from governance to design—should serve this purpose.
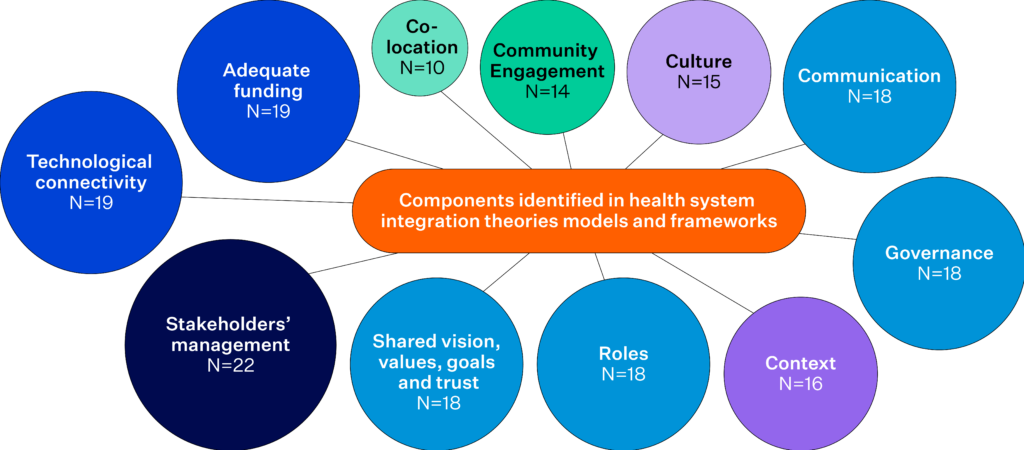
Since 2013, there has been a gap in literature regarding theories, models, and frameworks of health system integration.
Source: Piquer-Martinez, C., Urionagüena, A., Benrimoj, S. I., Calvo, B., Dineen-Griffin, S., Garcia-Cardenas, V., … & Gastelurrutia, M. A. (2024). Theories, models and frameworks for health systems integration. A scoping review. Health policy, 141, 104997.
Integration Is a Journey, Not a Destination
Health system integration isn’t something that can be ticked off a list. It’s an ongoing effort that requires visionary leadership, system-wide collaboration, and alignment across policy, technology, and clinical practice.
By approaching integration holistically, we can build platforms that enhance efficiency, improve health outcomes, and lay the foundation for sustainable healthcare systems well into the future.